According to the Centers for Disease Control and Prevention, COVID-19 deaths are up 10% from the previous week despite the overall infection rate falling by 1%. It has confounded researchers, then, why so few people are taking Paxlovid, the drug prescribed by doctors to counteract many COVID symptoms. In the peak of COVID-19 season, researchers are confounded as to why so few people are taking Paxlovid, the drug prescribed by doctors to counteract many COVID symptoms. According to a study by Pfizer, Paxlovid reduces hospitalizations from COVID by 86%.
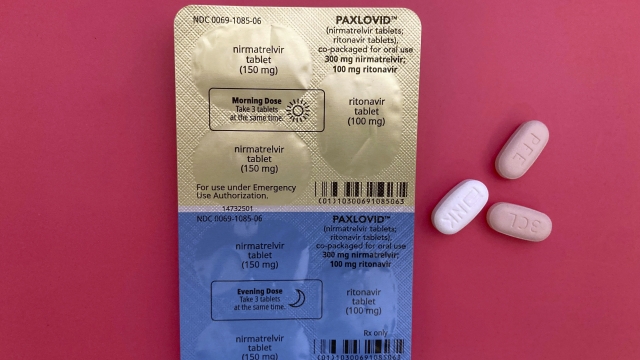
Paxlovid is an antiviral therapy that consists of two separate medications packaged together. The first is nirmatrelvir, which inhibits a key enzyme COVID needs to make more viral particles, and the second is ritonavir, which boosts nirmatrelvir's effectiveness.
A study from the National institutes of Health shows only 15% of people eligible for the drug actually take it.
“There are several factors that make doctors hesitant in prescribing this medication,” said Dr. Jaya Kumar, chief medical officer at Swedish Medical Center in Colorado. Dr. Kumar says Paxlovid must be taken within five days of symptom onset, otherwise it is ineffective. There have also been reports of rebound COVID infections ,and a foul metallic taste for those who have taken the drug.
Paxlovid is also expensive if insurance does not cover the cost, something that prevented Madelyne Maag from getting a prescription during her recent COVID infection.
“This was the most severe bout of COVID I’ve had to date,” she said. “I basically lived in the bathroom for the first three days. Heavy bouts of nausea, vomiting.”
It was Maag’s sixth time getting COVID. She said had she paid for Paxlovid without insurance it would have cost her $1,400.
“Right now I seem totally normal and fine, which is great,” said Maag. “But I’m worried because I didn’t have access to Paxlovid, what that’s going to look like in the next two, three, six months, 12 months. Is this going to be the COVID infection that gives me long COVID?”
Still, Dr. Kumar thinks considering the benefits of Paxlovid, it should be considered more seriously by those prescribed it.
“It’s a pretty effective drug,” said Dr. Kumar. “I do agree that it needs to be used more. But also, I feel like there need to be more studies, since all the studies were conducted before the newer variants came into being.”
SEE MORE: What living with long COVID is really like
Trending stories at Scrippsnews.com